When something is not working well or indeed at all, the primary goal is to find a way to repair it. The same thinking applies when that something is a someone, but often there is no fix or repair for a human being that works completely.
Historically, the mentally ill were subjected to inhumane treatment and locked away. Midway through the last century, the discovery of first-generation antipsychotic medication led to a new paradigm in the treatment of mental illness. By the 1960s, the process of deinstitutionalization was well underway and former “patients” were living in the community. Ideally, psychiatric care was to be provided within the community after deinstitutionalization; in practice access to care has been inconsistent with evidence suggesting “that fewer resources have been allocated to community-based services”.
The range of severity is wide; some people are able to manage their symptoms, while others cannot. Without the promised level of community support, those with serious mental illness often face struggles with addiction, unemployment, poverty, loneliness, and despair.
So, where do we go from here? It is clear that medication alone is not enough. A one-time repair is often inadequate to ensure a lifetime of wellbeing.
We need to change the focus from one of “fixing” an acute illness in the short-term, to one focused on creating a liveable life for the long-term, even if not all symptoms are resolved.
The Mental Health Commission of Canada states:
“The concept of “recovery” in mental health refers to living a satisfying, hopeful, and contributing life, even when a person may be experiencing ongoing symptoms of a mental health problem or illness. Recovery journeys build on individual, family, cultural, and community strengths and can be supported by many types of services, supports, and treatments.”
Internationally, and within Canada, recovery is seen as “key to achieving better mental health outcomes and improving mental health systems.” Recovery is intensely personal and relies on building a partnership between the person with mental illness and service providers.
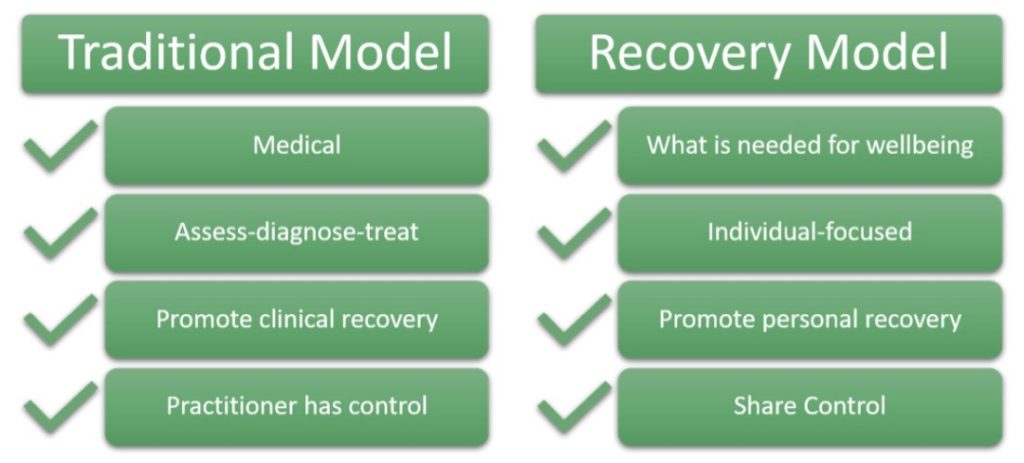
Based on a culture and language of hope, the recovery model creates supports with a person rather than for a person, promoting autonomy and power in decision-making. It is a paradigm shift that emphasizes the priorities and aspirations of the individual.
The recovery model is a holistic, person-centered approach to mental health care with 10 guiding principles (from SAMHSA’s working definition of the Recovery Model):
- Self-directed
- Individualized and person-centered
- Empowerment
- Holistic
- Nonlinear
- Strengths-based
- Peer support
- Respect
- Responsibility
- Hope
In the recovery model, professionals and patients form a supportive partnership working towards common goals. This is our vision for Eli’s Place.




