I didn’t have a physical medical problem per se. I reached out to my doctor for a psychiatric referral. But that was just one of my many unserved needs. I didn’t know my needs, nor how to navigate the maze of social services. Neither my doctor’s office nor society had a one-stop service to get me all the help I needed. I desperately needed a social prescription.

What Is Social Prescribing?
My social prescription might have linked me with a grief counsellor, advised me to contact the Distress Centre or even prescribed an art class or spending time in nature. I was lucky Victim Services connected me to a super occupational therapist.
Two things my social prescription would not include would be drugs or a referral to a psychiatrist. That remains my doctor’s domain. Social prescribing (SP) is a primary care service that links patients with non-medical needs to sources of support provided by the community and voluntary sector to help improve their health and well-being. Social prescribing is also called social care coordination. It is a holistic approach to personal healthcare: from treating the physically sick to preventative wellness. It integrates body, mind and social factors into the universe of social support services.
SP is currently being pilot tested in Ontario. The pilot introduces the concept of Ontario Health Teams (OHT); on each team link workers (also known as navigators) provide a one-stop service, diagnosing and referring patients to government and non-governmental offices, community and volunteer services. SP service providers could include a full community: social workers; psychologists; hospital discharge teams; dieticians; pharmacists; occupational, recreational, and physical therapists; housing and poverty services; and local cultural organizations. Social prescribing brings together health care and social services and moves us beyond the current and more limited ‘sick care’ model. It allows for better well-being and a more holistic approach to healthcare.

How It Works
A Commonwealth Fund study found that while 60% of family doctors screened for social needs, only 36% knew what social services were available in their community. The link worker’s role is to know and use that knowledge to collaboratively design a patient’s social care plan. The role of the link worker will now be part of each Ontario Health Team (OHT), which then orchestrates the service care plan. Electronic medical records will track the patient’s care journeys, results and engagement; reporting to the patient, doctor and social care providers.

The Benefits
Studies found patients are not comfortable discussing their non-medical needs with healthcare providers. Yet it is said that 80 to 90 percent of health and well-being is determined by factors outside of the mainstream of healthcare. SP empowers doctors, link workers, Ontario Health Teams, patients and social service providers to collaborate while co-designing care plans. A 2020 Alliance for Healthier Communities report found SP enabled a deeper integration of healthcare, interprofessional teams and social support.
Ontario patients report improved outcomes, a better sense of belonging, and confidence in self-managing their health. SP moves the focus from treating a patient to treating the whole person. My own journey through grief would have been far shorter and less needlessly negatively compounded were SP available four years ago.
De facto, SP de-medicalizes social care beyond the doctor’s office and hospital emergency services. Thus, SP reduces the time and expense of medical costs. In the UK, 59% of GPs believe SP helps reduce their workloads. After a year of the Ontario pilot, 90% of the participating doctors said SP improved their patient’s health and welfare. The United Kingdom SP program reduced emergency hospital admissions by up to 24%. Prescribed hobbies made patients more likely to recover from depression. And cultural engagements, such as prescribing art gallery tickets, lowered the odds of developing depression by 48%. SP addressed key areas of loneliness, isolation, food insecurity, and common interests. I deeply valued my weekly time with my occupational therapist for her counsel and companionship too.

Conclusions
We can look forward to this revolution in Ontario’s healthcare system and a healthier population. When you think about it, Eli’s Place will mirror aspects of social prescribing with its consolidation of psychological treatment and the social aspects of the working farm with its associated stores. The beneficial results of SP will bode well for 18 to 35-year-old participants with serious mental illnesses Eli’s Place seeks to serve.
Want to learn more about Social Prescribing, check out this video: What is social prescribing?
Eli’s Place will be a rural, residential treatment program for young adults with serious mental illness. To learn more about our mission and our proven-effective model click here.
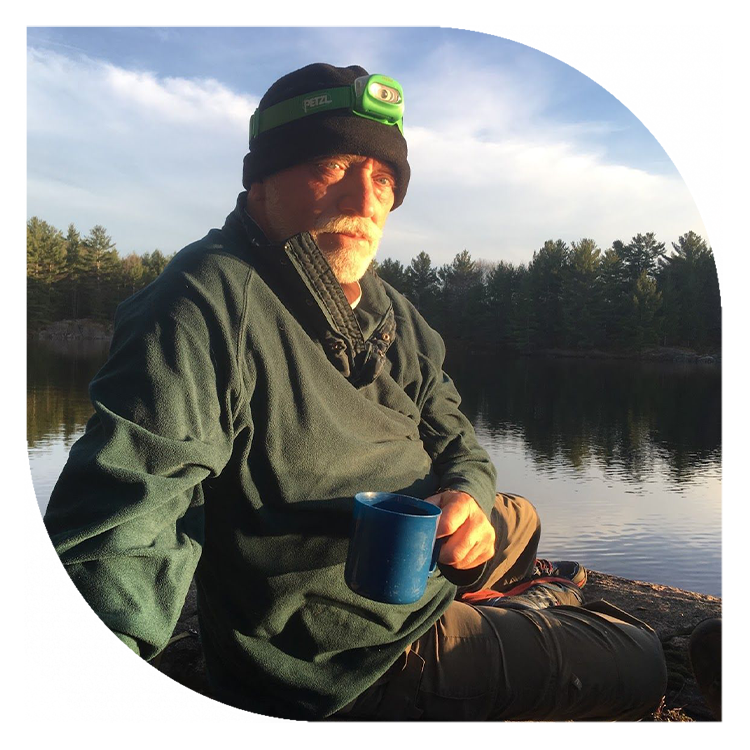
Richard Childs | Eli’s Place Volunteer
Father of the late Lucas, outdoors person, haiku and technical writer, and facilitator of organizational change. Grateful volunteer helping Eli’s Place come into fruition to save and enable young adult lives.




